Revenue Cycle Management (RCM) in healthcare is the backbone of a medical facility’s financial health. It ensures that healthcare providers receive timely and accurate payments for the services they offer. By streamlining administrative and clinical functions, RCM in medical billing optimizes cash flow, reduces claim denials, and improves overall efficiency.
What is RCM in Medical Billing?
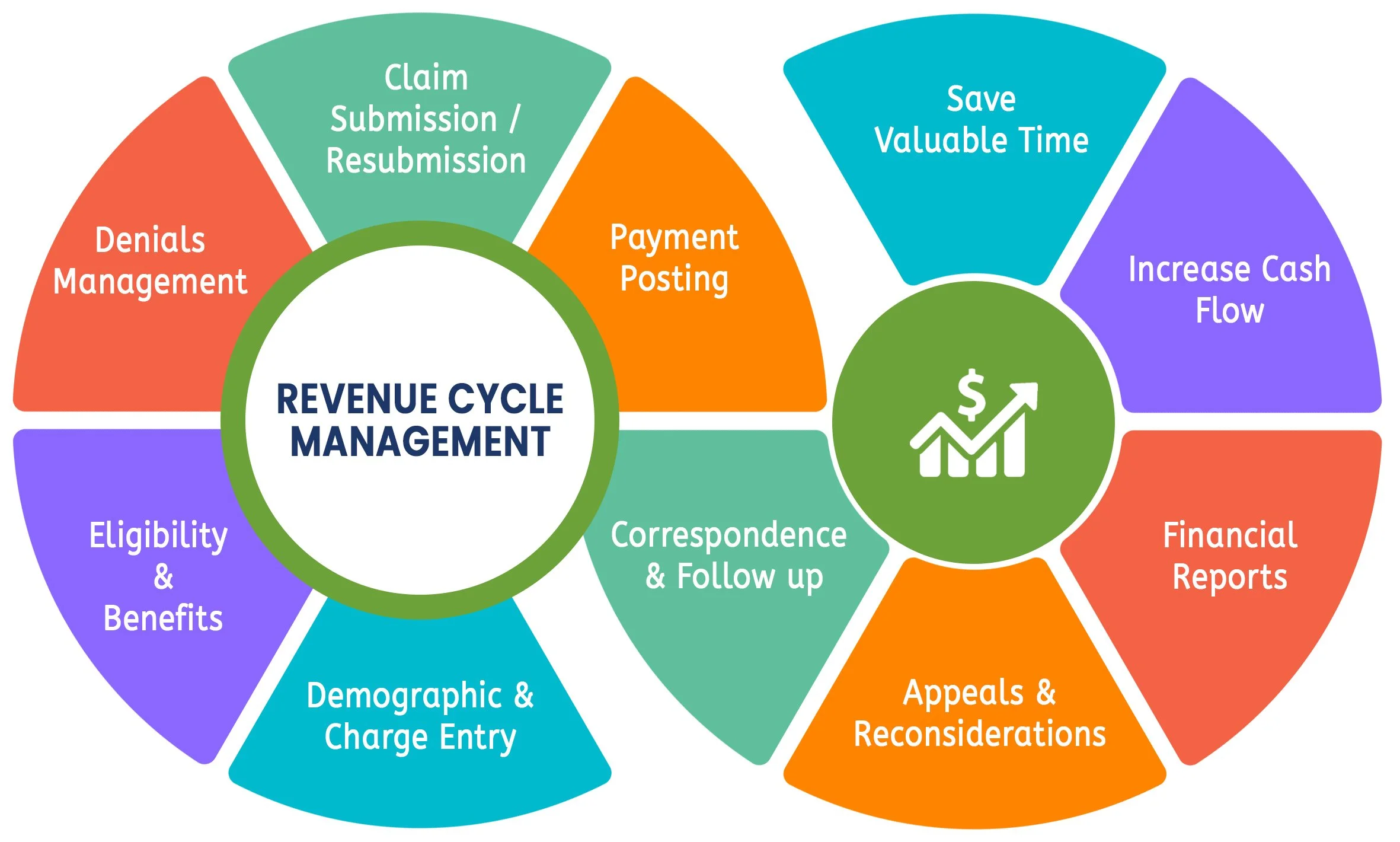
RCM, or Revenue Cycle Management, refers to the process of handling financial transactions related to patient care, from initial appointment scheduling to final payment collection. It involves multiple steps, including patient registration, insurance verification, claim submission, and reimbursement tracking. The goal of an effective RCM process is to minimize errors, prevent revenue leakage, and enhance the patient experience.
The Key Steps in the RCM Process
1. Patient Registration & Insurance Verification
The RCM process begins with patient registration, where accurate demographic and insurance details are collected. Insurance verification ensures that coverage is valid, reducing the risk of claim rejections. Accurate insurance verification is a crucial step in RCM in healthcare, preventing billing issues later.
2. Charge Capture & Medical Coding
Medical procedures and services must be properly documented and coded according to regulatory guidelines. Accurate coding is crucial to ensure that claims are submitted correctly and that providers receive appropriate reimbursement. Proper charge capture plays a significant role in the RCM process, ensuring no revenue is lost due to coding errors.
3. Claim Submission & Processing
Claims are submitted to insurance companies for review. Revenue cycle management companies often utilize advanced software to check claims for errors before submission, reducing the likelihood of denials and delays. Efficient claims management ensures a smooth RCM process, leading to faster reimbursements and fewer rejected claims.
4. Payment Posting & Denial Management
Once claims are processed, payments are posted to the patient’s account. If a claim is denied, the RCM team analyzes the reason, corrects any issues, and resubmits the claim promptly. A proactive denial management strategy within RCM in medical billing helps maximize revenue and reduce financial losses.
5. Patient Billing & Collections
After insurance adjustments, any remaining balance is billed to the patient. Effective RCM in healthcare ensures clear communication with patients about their financial responsibilities and offers options for prompt payment collection. Transparent patient billing practices strengthen trust and improve patient satisfaction.
Evaluate your practice today!
The Role of Revenue Cycle Management Companies
Many healthcare providers partner with revenue cycle management companies to handle their billing operations efficiently. These companies leverage advanced technology and industry expertise to streamline the RCM process, improve cash flow, and reduce administrative burdens for medical practices. Outsourcing to revenue cycle management companies can help healthcare organizations optimize revenue and improve operational efficiency.
Why is RCM in Healthcare Important?
An effective RCM system benefits healthcare providers and patients alike. It ensures that providers are paid accurately and on time while allowing them to focus more on patient care rather than financial management. Additionally, a streamlined RCM process enhances the patient experience by providing transparency in billing and reducing unnecessary financial stress.
Conclusion
RCM in medical billing is an essential component of the healthcare industry. From verifying patient insurance to managing claims and payments, a well-structured RCM process helps healthcare organizations maintain financial stability and operational efficiency. By partnering with revenue cycle management companies, medical practices can focus on delivering high-quality care while ensuring their revenue streams remain strong. A strong RCM in healthcare strategy is key to financial success and improved patient outcomes.